Data is critical for government to deliver effective, evidence informed policy. Data is important both for delivery of services (e.g. having people’s current contact details) and to allow government to understand what works. But the administrative path to getting data is not always straightforward.
Our work on boosting Human Papillomavirus (HPV) vaccination rates demonstrates how behavioural approaches can help.
The behavioural challenge
The Australian National Immunisation Program in Victoria involves all 3 levels of government. The Australian Government funds the program, the Victorian Government administers it and the vaccinations are delivered by local councils through secondary schools.
Schools hold the relationship with students and parents, and local councils rely on student and parent contact information provided by schools to record vaccinations. Without this information, it’s not possible for local councils to accurately track vaccination outcomes or send parents reminders to improve attendance on vaccination days.
HPV is a difficult virus to protect against. A vaccination rate of more than 80% is essential for reaching herd immunity against HPV. Achieving this will prevent many young Australians from developing cervical cancer in the future.
“This literally saves lives. There will be women alive in years to come because of the increased immunisation coverage being achieved today.”
~ Dr Brett Sutton, Former Chief Health Officer, 2019
What we did
We developed a communication intervention designed to encourage schools to share better quality data. We wrote a letter in plain language, included an action planning sheet, and sent these directly to school immunisation coordinators.
40 councils participated in the study, resulting in 307 schools in the trial (almost half of all secondary schools in Victoria). A randomised controlled trial was conducted where half of the schools in each council were randomly assigned to receive the letter and action planning sheet, and the other half didn’t receive anything. This allowed us to understand if an increase in data sharing could be attributed to the letter and action planning sheet.
Encouraging schools to share better quality data was the key step in achieving our goal of improving immunisation rates.
What we found
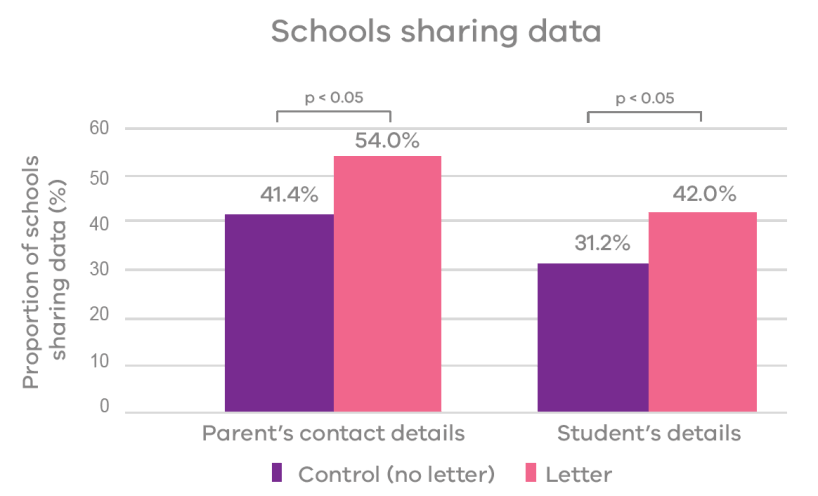
We found that more schools shared data when they received our letter and action planning sheet than did schools in the control group.
Related trials
Consent Card
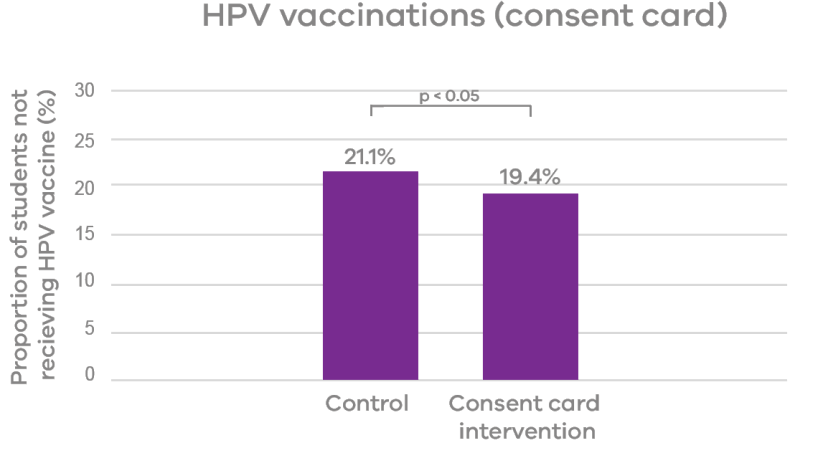
In a second trial we sent improved consent cards and a letter directly to schools. This intervention increased the likelihood of a parent or guardian returning the consent card by 3.5 percentage points, and increased the likelihood of the student receiving the HPV vaccine by 1.7 percentage points, bringing the share of unvaccinated students down from 21.1% to 19.4%.
SMS reminder
In a third trial we sent SMS reminders to parents when it was vaccination day at school. This reduced the share of students who had consented to immunisation but were not immunised from 14.3% to 11.0%. At scale, this type of intervention can get us past the last-mile of achieving full vaccination coverage for HPV.
What's next?
A behavioural insights approach is not just useful for understanding what works, but can also be used to enhance policy implementation. This trial shows that taking a simple step, like sending a letter and action planning sheet, can result in government receiving better quality data which in turn helps government improve outcomes for Victorians.
Behavioural insights-informed communications have significant potential for helping to improve policy implementation.
Thanks
We thank our partners the Department of Health and Human Services, BehaviourWorks Australia and the Public Sector Innovation Fund.
Updated